Introduction
Ovarian stimulation aims to obtain the maximum number of quality eggs. However, since we do not have a way to assess the intrafollicular egg to track its quality, we monitor the follicle with an underlying assumption that its property, size, and estradiol production in some way reflect the quality of the oocyte. However, once the cavity has formed in the follicle and the egg’s growth factors become too diluted to control distal cells, mural granulose escapes the egg’s control and differentiates with the expression of FSH receptors. Therefore, when the follicle is recruited into the follicular phase, the egg and its follicle are in pending “divorce,” where the egg only controls nearby cells, the so-called cumulus. In contrast, follicle size and estradiol production are controlled by FSH. Therefore, follicle size and estradiol level provide little information about the egg.1 This explains why all data demonstrate a weak association between the follicle’s parameters per se and the egg’s competency. This association does not seem stronger than that between the circumference of the pregnant woman’s abdomen and the maturity of the fetus inside. Therefore, we proposed a hypothesis that the duration of the follicle’s “pregnancy” with the egg is a better benchmark for the egg’s competency, similarly to the duration of pregnancy being a better benchmark for fetal maturity. To keep terminology in line with obstetrics, we named this duration – Term Follicular Phase or Term Stimulation when applied to the controlled cycle.2
We proposed that the duration of Term Stimulation must be close to the duration of the follicular phase seen in the most fertile female population, about 17 days before LH surge.3 Term Stimulation extends ovarian stimulation to the physiological duration of the follicular phase seen in the most fertile patients’ population by maintaining FSH levels in circulation within predefined limits (Dozortsev and Diamond, JIVFww, submitted). Due to the novelty of this approach and a considerable amount of additional effort involved in the Term Stimulation cycles, it is currently reserved (with some exceptions) to only those cases when the patient had at least two previous attempts of IVF, which failed due to either poor embryo quality or gross chromosomal errors, and who refuses to consider donor eggs option. Even though chromosomal errors are found in well-developing embryos, they originate during first or second meiotic division and usually reflect low egg quality.
When reading case reports, it is important to bear in mind given the limited physician experience with Term Stimulation, many decisions about the FSH dosage are made empirically and intuitively. This is why, for example, in the first case, the administered amount of FSH increased on day 15, or in the second case, the initial dose of FSH was set at 300 IU.
Cases reports
First case
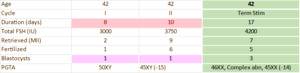
The first case describes a patient 42 years old, BMI 30, AMH 1.13 ng/ml, G0, P0 with two prior failures of IVF due to the lack of chromosomally normal embryos. Table 1 summarizes her three IVF attempts. The attempts were similar in all aspects, except the monitoring and administering FSH – Term Stimulation method.
The target duration of stimulation was set to 17 days, calculated from the first day of the period. Based on the patient’s baseline FSH, her target serum FSH level was set to the range between 15 and 20 mIU/ml. Ovarian stimulation was initiated on the second day of the menstrual cycle. The amount of FSH for administration was calculated to achieve and maintain the circulating level within this band. If the circulating FSH level deviated from the band, the amount of injected FSH was adjusted accordingly. Table 2 summarizes the Term Stimulation cycle.
Once the set 17-day duration of the follicular phase was achieved, hCG was administered to trigger ovulation. Seven eggs were retrieved, of which 5 were mature and inseminated with ICSI, and 3 fertilized oocytes developed to the blastocysts stage (Table 1). Blastocysts were biopsied and frozen. Subsequently, one chromosomally normal blastocyst was transferred in a frozen cycle, resulting in a singleton pregnancy, which at the time of writing is at 22 weeks, progressing uneventfully.
Second case
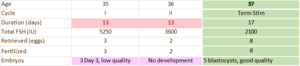
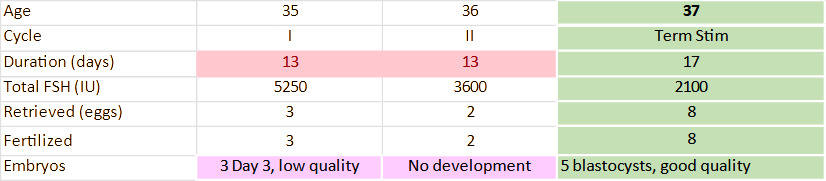
The second case describes term stimulation in a 37-year-old patient, AMH 1.87 ng/ml, BMI 29, G0, P0, with two previous IVF failures due to poor embryo quality. Table 3 summarizes her three cycles, including Term Stimulation. The attempts were similar in all aspects, except the monitoring and administering FSH – Term Stimulation method.
The target duration of stimulation was set to 17 days, calculated from the first day of the period. Based on the patient’s baseline FSH, her target FSH level was set to 5 and 10 mIU/ml. Ovarian stimulation was initiated on the third day of the menstrual cycle. The amount of FSH for administration was calculated to achieve and maintain the circulating level within this band. If the circulating FSH level deviated from the band, the amount of injected FSH was adjusted accordingly, including coasting on days 10 and 14. Table 4 summarizes the Term Stimulation cycle.
Once the 17-day duration of the follicular phase was achieved, hCG was administered to trigger ovulation. Eight mature eggs were retrieved, all fertilized, and five developed into good-quality cryopreserved blastocysts (Table 3). Subsequently, two blastocysts were transferred in a frozen cycle, resulting in a singleton pregnancy and uneventful term delivery.
Discussion
The presented cases demonstrate that, at least in some instances, extending the follicular phase to “term” provides the opportunity for achieving pregnancy in cases with poor egg quality. In a context of concern that high FSH levels may adversely affect egg quality, it is interesting that in the first case, the total amount of used FSH was slightly higher in the Term Stimulation cycle than in prior conventional cycles. However, the average daily dose of FSH in the Term Stimulation cycle was lower (263 IU vs. 375 IU). This may indicate that the adverse effect of FSH,4 if it exists, is mediated not by the total amount but by its peak concentration. In the second case, the yield of eggs was higher despite the smaller amount of FSH used in the Term Stimulation. This is typical for Term Stimulation cases.
In both cases, the stimulation lasted for 17 days (counting from the first day of the cycle); however, depending on patient-specific circumstances, it can be shorter or longer. It is important to note that in cycles with extended stimulation, the risk of spontaneous, LH-independent follicular luteinization increases. We mitigate it with diclofenac, usually vaginal suppositories, 50 mg twice daily.
In both presented cases, the stimulation was performed in a natural cycle, but it can also be performed in cycles primed with birth control pills.
Irrespective of Term Stimulation’s ability to achieve pregnancy, it represents a new level of control over the cycle, where instead of “chasing the size of the follicle,” we can determine the trigger and retrieval date before the stimulation even begins. We hypothesize that after about 1000 cycles, it will be possible to take advantage of artificial intelligence to assist physicians by administering Term Stimulation using a combination of FSH and E2 measurements without or with only a minimal number of pelvic ultrasounds, making it highly scalable and “portable,” more convenient and less expensive.5
Authors’ Contribution per CRediT
Conceptualization: Dmitri Dozortsev, Michael Diamond; Methodology: Dmitri Dozortsev, Lina Villar; Formal analysis and investigation: Lina Vilar, Dmitri Dozortsev, Israel Maldonado; Writing - original draft preparation: Lina Villar, Dmitri Dozortsev; Writing - review and editing: Dmitri Dozortsev, Lina Villar

.png)
.png)

.png)
.png)